“The healthcare of tomorrow is customer-centric, distributed, and value-driven and leveraging technology to its full potential is key,” said Jennifer Mueller, VP of Data and Privacy with the Wisconsin Hospital Association in a recent presentation at Hyper Innovation’s Challenges in Health Tech Series. Mueller underscored some of the key challenges to address in healthcare that technology can solve for:
- Changing consumer expectations and behaviors around provider care and data
- Aging population and lagging population growth
- Aging workforce as baby boomers retire in record numbers in the coming years
- Workforce shortage with lack of new healthcare staff entering the workforce at a rate comparable to looming the retirement population
- Provider burnout from documentation and lack of care team support (see workforce shortage)
- Under-utilization of technology and data integration to relieve burden and create efficiencies in care
Healthcare Models Are Changing
Healthcare models are changing and providers need to make fundamental changes in order to keep up with the ways consumers want to receive care. With the growing use of fitness trackers and remote devices, consumers are in charge of much of their own data and are pushing for engagement that traditional systems are unable to provide.
Aging Population and Workforce
By 2032 the population over 75 will grow by 75%; the population under 18 will grow by only 3.5%. Wisconsin’s population older than 65 will double by 2030 and health care demand will increase by 30%. This “silver tsunami” drives the importance of adopting new models of care:
- Value-based care models for patient-centric care, including transparency in care to better communicate with patients
- Increased efficiency in documentation to reduce provider burden and time spent away from patients
- Automation of prior authorizations to speed up the time between care procedures and reduce healthcare staff burden
- Integration of telemedicine, remote patient monitoring, and virtual care into healthcare models and data flow
Value-Based Care Models
“Healthcare models need to move from fee-for-service to value-based care in order to maintain consumer participation and provide maximum value,” said Mueller. This style of care, with incentives and revenue models around keeping healthy people healthy and out of the clinic, will bring the most value to systems and payers by way of improving patient outcomes and lowering cost of care.”
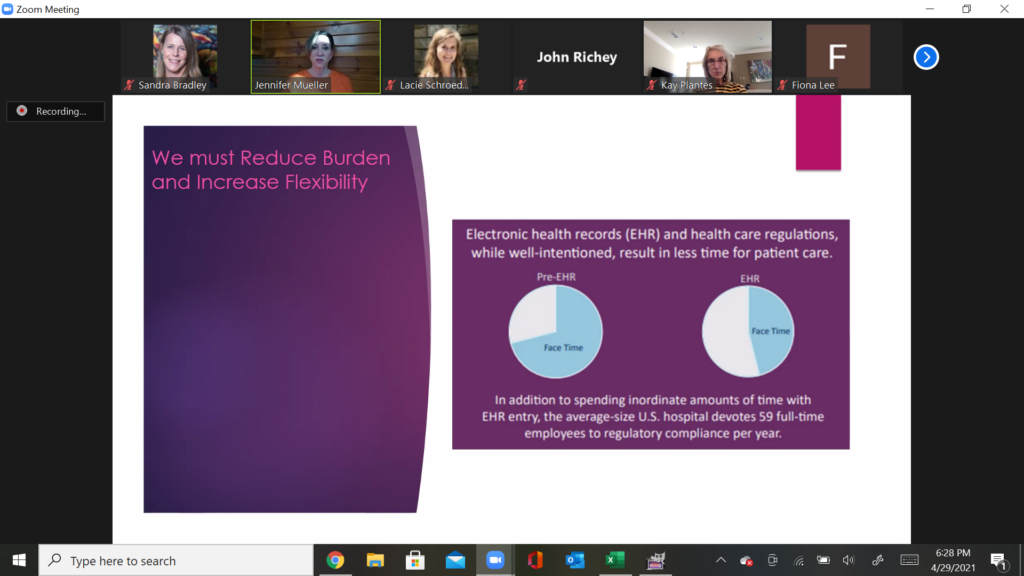
Reducing Provider Burnout
“We know that U.S. clinicians are spending more time in the electronic health record than they are with patients. We must reduce burden on our health care workforce,” said Mueller.
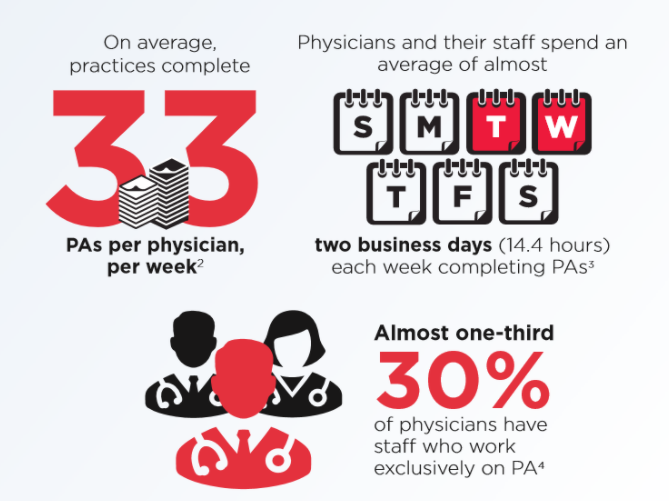
Mueller used the example of Prior Authorizations (PAs) as an example of a process needing innovation. “The burden on our providers is very large. Payers are trying to control costs by reviewing documentation to ensure medical necessity, but the volume of these requests over time have dramatically gone up.”
Leveraging Technology and Data
Healthcare models need to change to meet needs for clinicians to better manage patients and to meet growing market needs.
While the pandemic “jumpstarted” the adoption of technologies including telemedicine and remote patient monitoring, there are gaps in fully operationalizing digital tools to address key challenges.
To address key challenges in healthcare that technology can solve, Hyper Innovation invites campus innovators and students to ideate and propose solutions in the Hyper Innovation Digital Health Challenge this summer. The Challenge is designed to connect real-world industry problems to solve to university innovators and entrepreneurs.